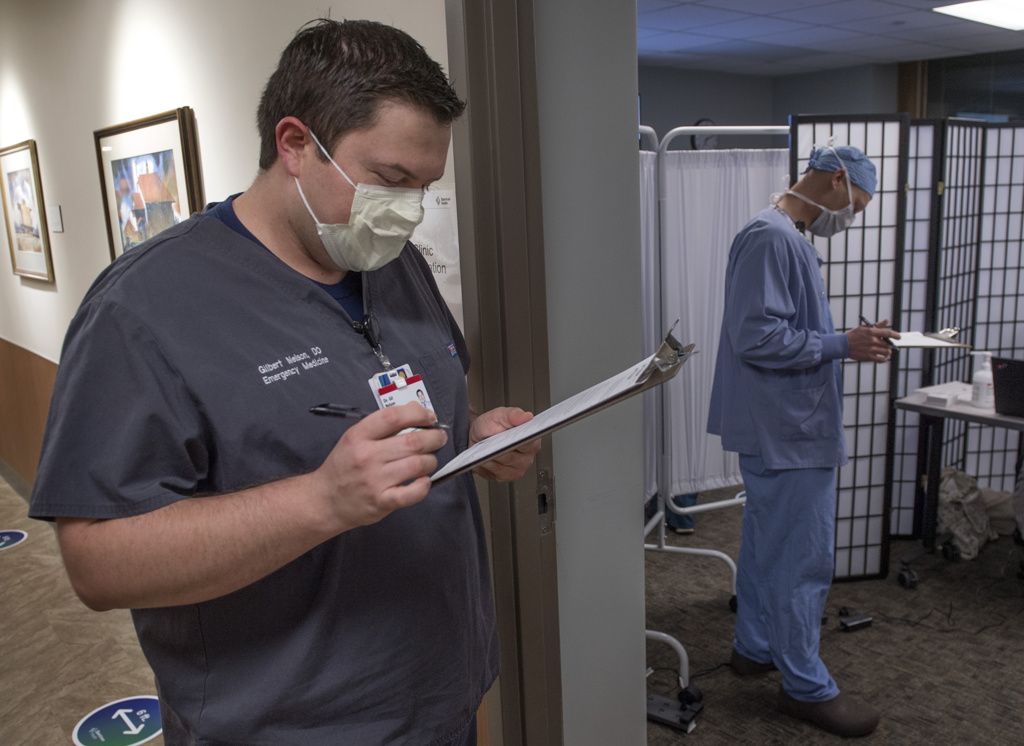
Gil Nelson, DO, sat down and rolled up the sleeve of his medical scrubs for his COVID-19 vaccine.
“That wasn’t too bad at all,” he said, as nurse Laurie Sayer, RN, delivered the injection into his upper arm.
Dr. Nelson, an emergency medicine resident physician, was among team members who received the vaccine at a clinic at Spectrum Health Butterworth Hospital last week.
“Driving in today, I felt pretty fortunate that I would be getting this so early,” he said.
In the emergency department, Dr. Nelson treats patients with COVID-19 every day.
“It is definitely a unique virus—with the long-lasting effects it can have on some people,” he said.
He and his wife, Sara, have three daughters. When he received a call over the weekend scheduling his vaccination, they received the news with relief.
“It will give a little more peace of my mind—to me and my family,” he said.
Although Spectrum Health team members are encouraged to get the vaccine, it is not required at this time.
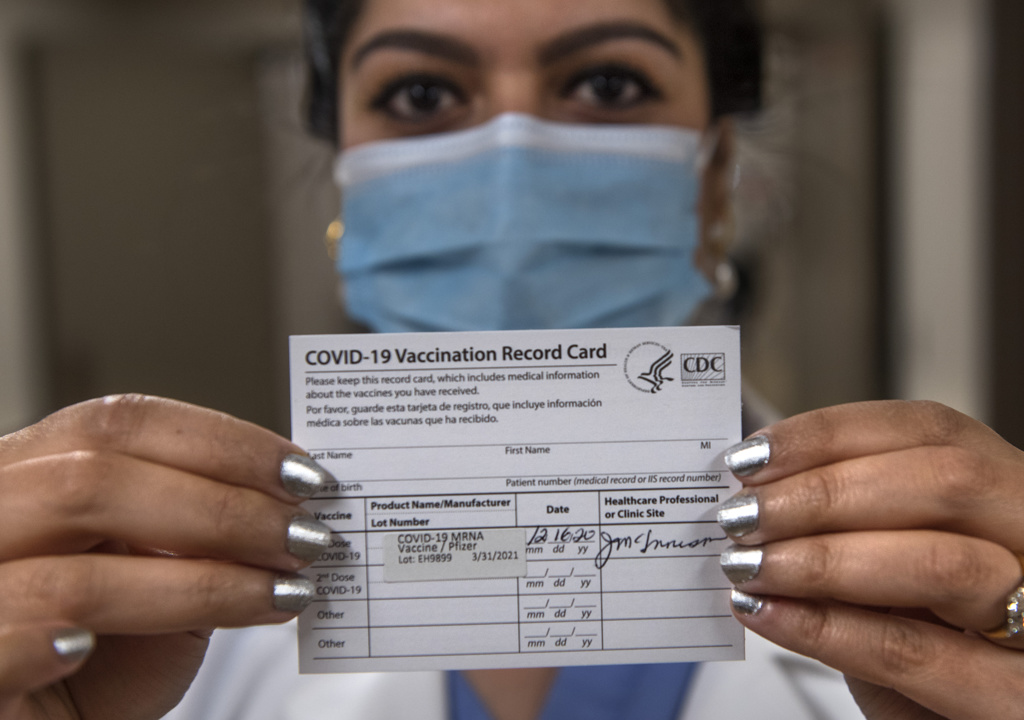
The first COVID-19 vaccine, produced by Pfizer, received emergency use authorization from the U.S. Food and Drug Administration on Dec. 11.
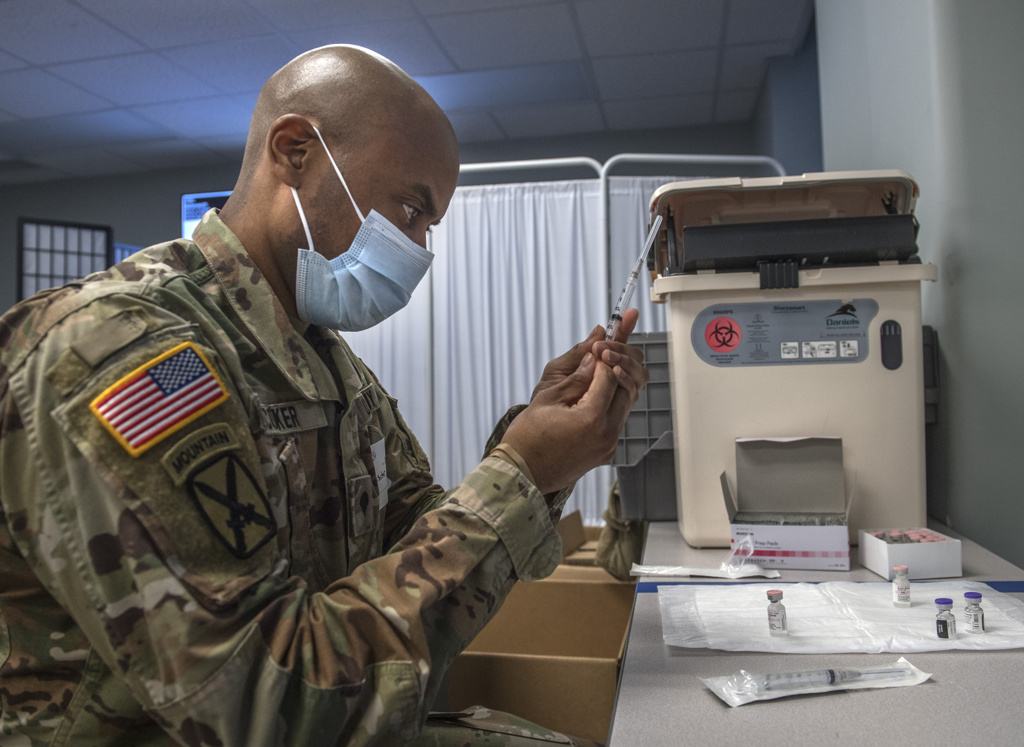
Spectrum Health received its first shipment of the vaccine on Dec. 14. Five medical team members received the first vaccines at noon that day.
One said he had mild chills and a mild headache an hour after receiving the vaccine. The others said they had only mild arm soreness where they received the injection.
Federal guidelines call for health care workers and residents of long-term care facilities to receive the first shots.
At Spectrum Health, the scheduling of vaccinations prioritizes health care team members who have the most significant risk of exposure to COVID-19, such as those who work in the emergency department and intensive care units.
Vaccination clinics for team members began last week at Butterworth Hospital, Big Rapids Hospital and Lakeland Medical Center. As supplies of the vaccine allow, clinics will be scheduled at other Spectrum Health hospitals.
‘This is a great day’
Arriving at the clinic at Big Rapids Hospital, Lauren Pasche, RN, described the vaccine as a positive step forward in the fight against COVID-19.
“I want to be a part of the solution to this horrible pandemic,” said Pasche, a nurse at Big Rapids Hospital and Reed City Hospital. “I’ve seen a lot of death and suffering over the last nine months, so I am very excited to get the vaccine today.”
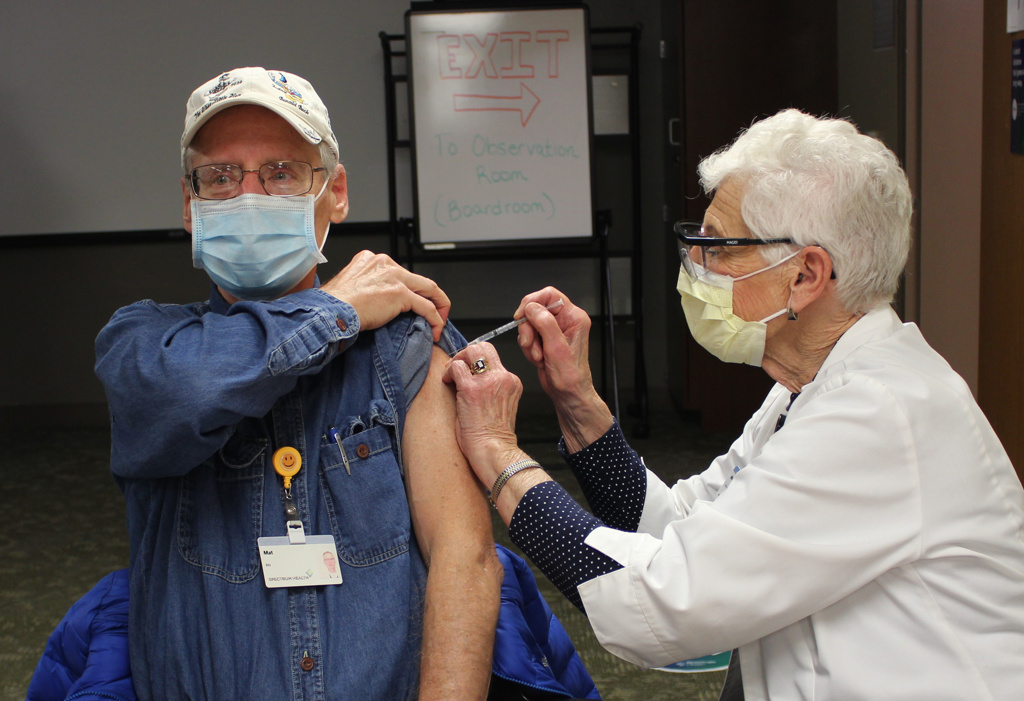
Mat Wellnitz, RN, a nurse at the Big Rapids Hospital ICU, thought about the impact of the vaccine on the broader community.
“I grew up in this community— this is my town,” he said. “I think it’s important for me to show other people that it is safe and hopefully this will inspire people to say yes, it’s OK to get it.”
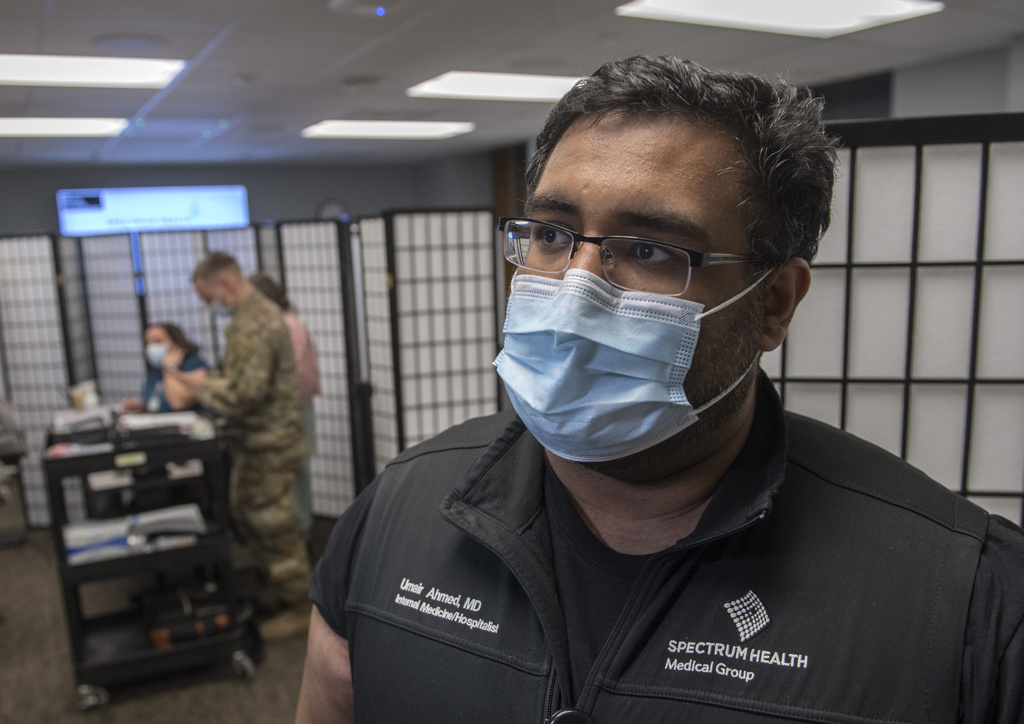
After enduring a bout with COVID-19, Umair Ahmed, MD, felt eager to get the vaccine.
“I don’t want to go through that again,” he said. “It was the sickest I have ever been in my life by far.”
Dr. Ahmed, an internal medicine physician at Butterworth Hospital, said his illness started in April with gastrointestinal symptoms.
He later developed body aches and respiratory symptoms, including a cough and shortness of breath.
As his blood oxygen level dropped into the upper-80% range, he worried he would need hospitalization. After receiving steroids, his condition improved.
“By day 12 to 14, I felt 90% better,” he said. “But I was pretty miserable for those two weeks.”
As a hospitalist, Dr. Ahmed admits patients to the hospital. These days, about a third of those admitted have COVID-19, he said.
He draws on his experience to provide patients hope for recovery. He lets them know, “We do have treatments. People do get better.”
Dr. Ahmed welcomed the vaccine because he worries about the chance he could be re-infected with the virus.
And he hopes it will be a turning point for the country as it battles the contagious virus.
“We are seeing hope—a light at the end of the tunnel,” he said.
A turning point
Tyler Wooldridge, RN, a nurse in the cardiothoracic intensive care unit, suffered from COVID-19 in September.
“I had all the symptoms, and I was sick for 10 days,” he said.
The most difficult symptoms were the cough and loss of his sense of smell and taste.
“Soup tastes like hot water,” he said. “And you can feel the salt on something, but you can’t taste it.”
When a scheduler called him about a vaccine, Wooldridge said, “I was excited. I’ve been waiting all year for it.”
Like many others, he has canceled vacations and taken precautions to reduce the spread of the virus.
“I’m ready for normal life,” he said. “I’m a traveler. I like hanging out with my friends.
“I would like to go to Florida and sit on the beach—or just go somewhere nice.”
Working in neurocritical care, Tia Chakraborty, MD, cares for patients with COVID-19 as well as those with brain injuries from strokes, aneurysms, seizures and other neurological issues.
Her heart goes out to patients hospitalized during the pandemic. Because of visitor restrictions to prevent the spread of COVID-19, some patients cannot have family members by their side. That makes difficult discussions about medical care, and even end-of-life decisions, more difficult.
“The nurses have been so amazing about holding their hands and relaying messages of love from their loved ones,” she said. “But it has just been trying for everybody.”
Dr. Chakraborty and her husband, Paul Berglund, are vigilant about following public health guidelines to reduce the spread of COVID-19. But she knows her husband and parents worry about her because she works in health care.
When she received her injection, Dr. Chakraborty pulled out her phone to take a picture—to provide proof for her worried mom.
She is impressed by the research that went into the vaccine and the data from the clinical trials.
“I had no doubt whatsoever about getting it,” said Dr. Chakraborty, a neurologist. “I was thrilled when I got the call Saturday to schedule it.”














 /a>
/a>
 /a>
/a>
 /a>
/a>