Kevin Farhat, 56, admits he’s a lucky man.
On Jan. 11, he suffered a severe headache—later described as a thunderclap headache—and neck pain radiating down his back.
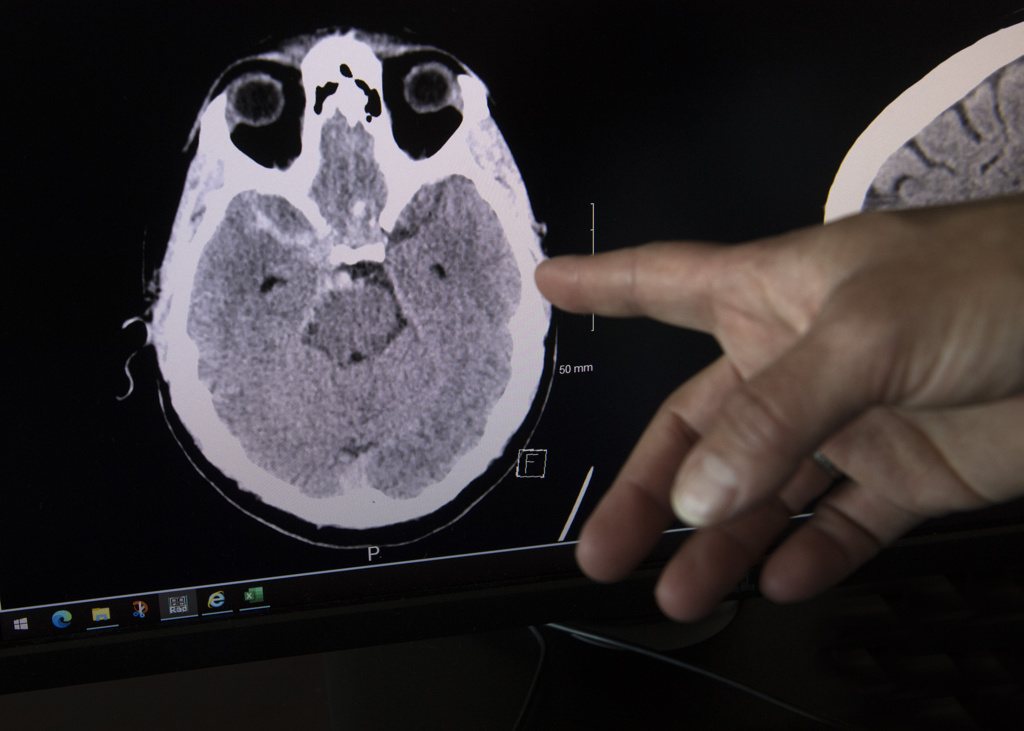
The excruciating pain brought him to his knees. He managed to call a friend for a ride to Spectrum Health Butterworth Hospital, where he quickly underwent a CT scan.
The health team identified the problem—a burst aneurysm and a stroke.
Farhat needed immediate surgery.
His experiences were common for someone who suffers a burst aneurysm followed by a stroke, said Paul Mazaris, MD, a cerebral vascular neurosurgeon with Spectrum Health.
About 1 in 3 people who suffer an aneurysm and stroke won’t make it to the hospital alive. Those who reach the hospital, however, stand a good chance of survival.
Recovery is a team effort.
Dr. Mazaris and his surgical staff lead the initial care, which is immediately followed by treatment in the intensive care unit.
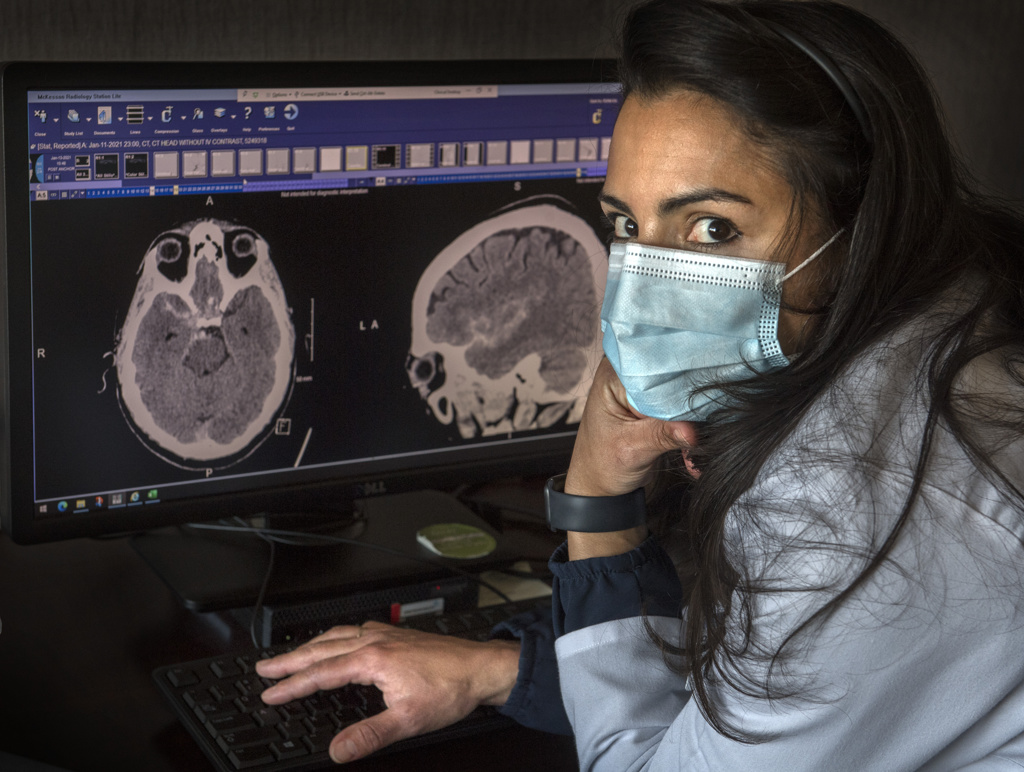
“It all happens very quickly,” said Hilda Guerra, MD, a specialist in neurocritical care at Spectrum Health. “It takes a team of physicians and assistants, respiratory therapists and nurses working very fast to take care of these patients.”
Dr. Guerra leads the treatment in the intensive care unit.
“There is a lot going on whenever there is a bleed or stroke,” she said.
The decision to perform brain surgery must be made within 24 hours of the burst aneurysm or stroke.
Surgery itself is relatively low risk, although it can take several hours, Dr. Mazaris said. His team includes physician assistants Leah Lyons and Taleen Mergian.
The extent of the damage done by a rupture is a significant factor in determining survival and recovery, although a patient’s age and health are also factors. Younger, healthier patients stand a better chance of recovery.
Quick response
Following surgery, Farhat spent about two weeks in intensive care.
Dr. Guerra, a neurointensivist, specializes in treatment for severely ill patients. This usually involves patients with blood clots in the brain, brain bleeds and aneurysm ruptures.
Sometimes, a patient will go straight from the emergency department to Dr. Guerra, who could determine if surgery is needed. But there are also times when emergency department doctors call the surgeon.
Ultimately, any patient battling a brain bleed will come under Dr. Guerra’s care.
She follows the patient throughout the health journey, ensuring their vital organs are operating properly and guarding against organ shutdown.
The intensive care team performs a myriad of critical functions.
“We put in breathing tubes, central lines, big IV lines,” Dr. Guerra said. “We do a variety of procedures to treat patients depending on what type of brain problem and side effects they are experiencing.”
Fortunately, many of the medical challenges in the intensive care unit are predictable and treatable.
“We know what to expect and how to treat them to keep them alive and prevent other medical problems,” Dr. Guerra said. “We manage things very tightly so people don’t develop complications.”
Life changes
Farhat returned home after 14 days in intensive care.
Although he wasn’t necessarily in poor health before the aneurysm burst, he’s already working to make a number of changes to ensure a full recovery.
Before this experience, he hadn’t seen a physician regularly. That will change, he said.
He also plans to attend all follow-up appointments.
He’s cutting out alcohol and has stopped smoking. He’s working to reduce his salt and sugar intake. He plans to eat a high-protein diet and stay away from fried foods, burgers and similar fare.
“All of the things I enjoyed a few months ago,” he said.
He’s getting more rest, too.
He owns three bars in the Grand Rapids area, but has trimmed his own work hours drastically—from the typical 70 hours a week to about 25.
He recognizes that many people die from what he went through. It’s a blessing not only to be alive, but to be alive without any major side effects.
“I’m very, very lucky,” he said. “Based on what I’ve read about what I had, I could have been looking at six to eight months of recuperating, possibly on a feeding tube and a ventilator.”
He has plenty of family to enjoy, including a brother, three sisters, two nephews and a niece.
“I have a lot to live for,” he said. “I’m pretty successful and I have a lot of people who are praying for me and those prayers obviously help.”
He also credits what he calls an incredible medical team.
“I’m grateful to be living in a city that has this level of neurosurgery expertise,” he said. “In my opinion, it’s second to none.”













 /a>
/a>
 /a>
/a>
 /a>
/a>