For years, David Ronk worked on the third floor of an office building in Jackson, Michigan. Several times a day, the engineer and corporate executive made a point of taking the stairs.
But sometime in 2018, he could no longer keep up this routine.
“I began to notice that I was having difficulty climbing stairs,” he said. “It got to the point where if the elevator was available, I’d take the elevator. And then it got to the point where even if the elevator wasn’t available, I’d wait for it.”
David underwent tests and imaging, and soon received a diagnosis: idiopathic pulmonary fibrosis, a progressive disease of unknown cause that scars the lung tissue and interferes with oxygen delivery to the body.
Though medications can provide temporary relief, David didn’t have much hope for the long term.
Three-year decline
In April 2020, David retired from his job.
His breathing difficulties soon began hampering his ability to do projects around his family’s East Lansing home.
As the illness progressed, he developed a chronic cough and intermittent swallowing issues—both symptoms of worsening pulmonary disease.
He and his wife, Cheryl, became increasingly concerned. Early in 2021, with no remedies in sight, he looked into the prospects of a lung transplant.
He learned about the transplantation process and his options—there were three lung transplant programs in Michigan, he said, plus several out of state.
He received a referral to one of the programs, but soon received a letter declining his case based on his age—two months shy of 68 years.
Six months passed.
Cheryl, who had taken on the role of coach and caregiver, encouraged her husband to keep up his strength despite constant fatigue.
“He would get up, he’d get dressed, he’d come downstairs … and he’d sort of just fold into this big leather chair and read the newspaper and watch TV. That was it. I mean, he couldn’t do much else,” she said.
“But I made him do those steps—upstairs and downstairs. … I wouldn’t give up on that.”
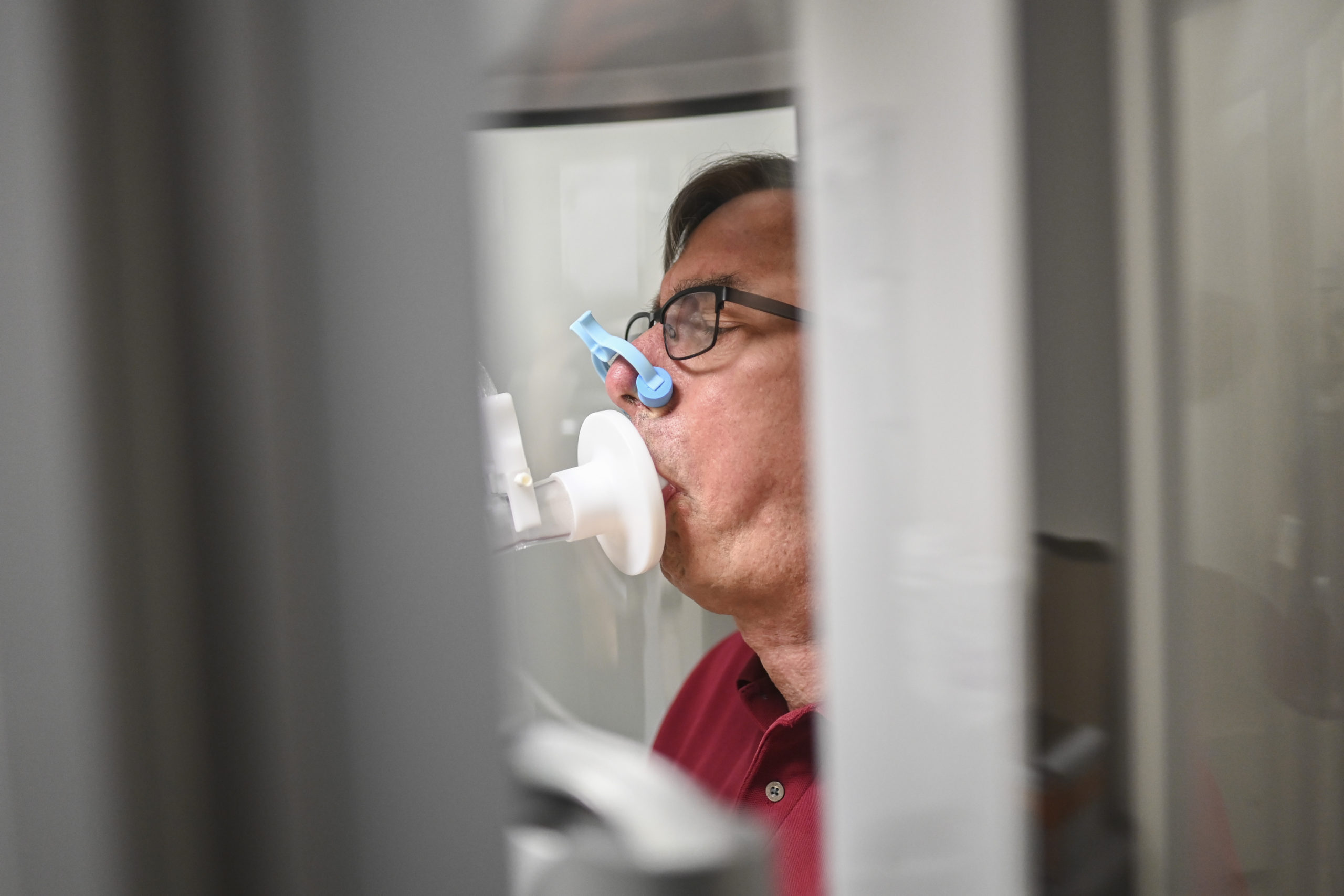
In August 2021, David began requiring supplemental oxygen to support his breathing. He also inquired about a referral to another lung transplant program.
“It was within a week or so after that visit that I was contacted by Spectrum,” he said.
That phone call marked the start of a brighter future.
But the Ronks have since learned—and they want others to know—that patients can contact lung transplant centers directly. They don’t have to wait for a referral.
Lung transplant list
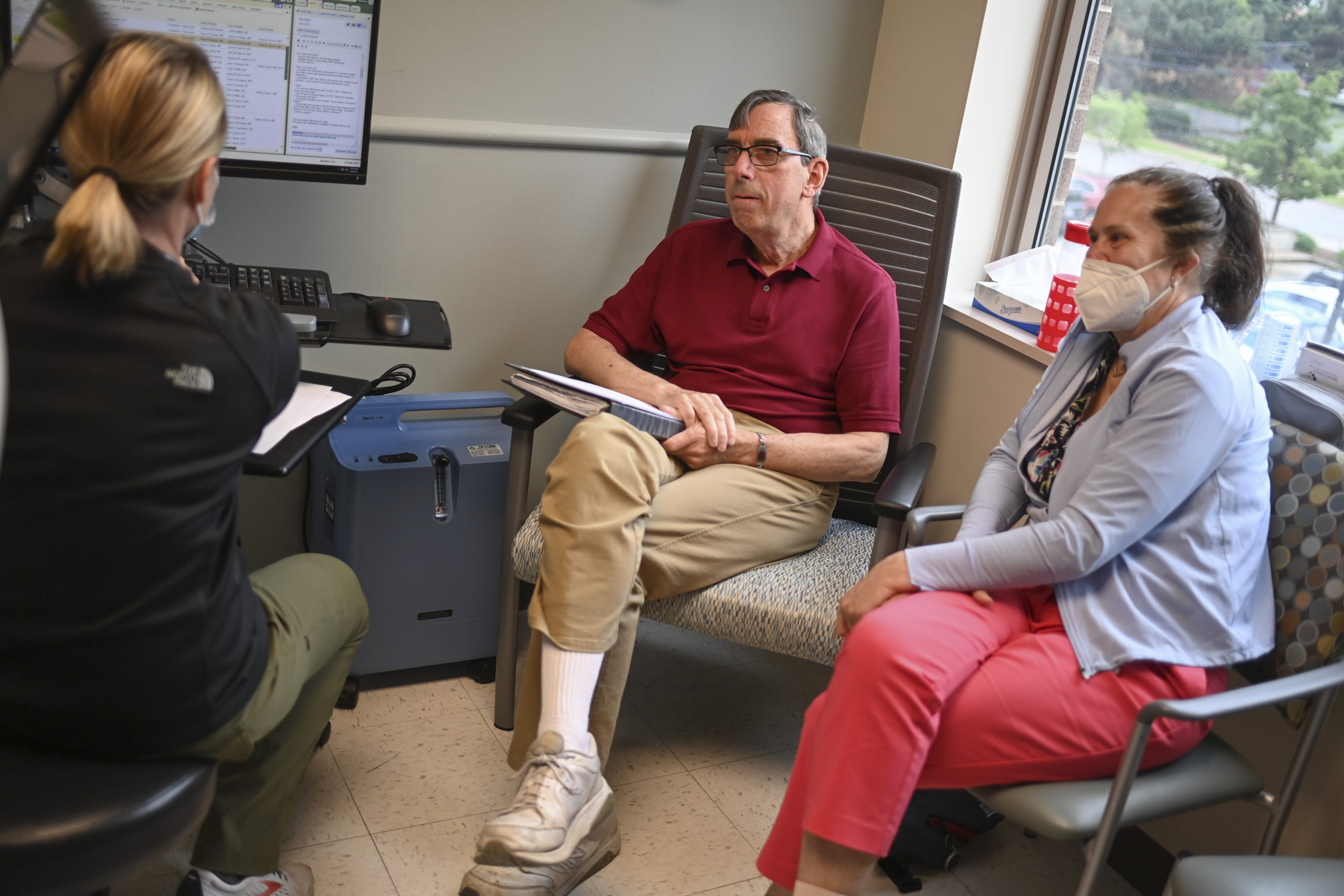
David and Cheryl had their first meeting with the Spectrum Health Richard DeVos Heart and Lung Transplant Program that fall.
The pulmonology team performed an initial examination, reviewed David’s medical history and, despite his age and weakened state, offered to get him started on the program’s extensive pre-transplant evaluation process.
Caitlin Kothe, RN, his pre-transplant coordinator, characterized the couple’s initial visit as a last-ditch effort.
“They were preparing basically for end of life at home,” she said.
Pulmonologist Ryan Hadley, MD, recalls working with David during the testing and evaluation phase.
“The thing that really struck me is how hard the disease had hit his body,” Dr. Hadley said. “He may not have been a candidate at many other centers just from how much strength he had lost.”
And yet, by the end of the evaluation process, the transplant team felt comfortable recommending David for bilateral lung transplantation.
Edward Murphy, MD, the surgical program director for lung transplantation, said David’s relatively simple medical history and Spectrum Health’s strong track record gave the team confidence he could do well after surgery.
“Despite his age, he really—he didn’t have other significant medical problems. … He was a never-smoker and didn’t have an extensive past medical history,” Dr. Murphy said.
“Some patients are in their upper 60s or even 70s and are perfectly suited for lung transplantation—and to deny them that opportunity is unnecessary, because we have excellent outcomes with patients regardless of their age.”
Because of its highly skilled team, the Spectrum Health program often accepts patients other centers might turn away, Dr. Murphy said—including patients on an ECMO machine, those who have coronary artery disease, even those who’ve undergone previous lung transplantation.
David got the green light for his transplant—and a spot on the UNOS waitlist—just before Thanksgiving 2021.
Not knowing whether David’s wait would be days or months, Kothe advised the Ronks to be ready to leave for Grand Rapids at a moment’s notice.
“She told me at that point, ‘Cheryl, make sure that you’re packed. This could even happen this weekend.’
“I kind of didn’t believe it and thought, ‘That’s what she says to everyone,’” Cheryl said.
But she packed a bag just in case and made plans for a quick departure.
Less than a week later, on an afternoon in early December, David’s phone rang.
It was the Spectrum Health Lung Transplant Clinic—he had been matched with a pair of donor lungs.
Astonished, Cheryl packed up her laptop and loaded the car. With an oxygen cylinder bungee-corded into the backseat to support David’s breathing en route, she helped him into the passenger seat.
Less than a half-hour after receiving the call, the couple pulled out of the driveway.
Ex vivo lung perfusion
Meanwhile, at Spectrum Health Butterworth Hospital, lung transplant team members were coordinating logistics related to David’s donor lungs.
Because the offer for the matching lungs came on very short notice, Spectrum Health didn’t have time to send a surgical team to the donor site to personally evaluate and retrieve the lungs—the normal method of procuring lungs for transplantation.
Instead, a surgical team at the donor hospital removed the lungs and arranged to transfer them to a nearby company that specializes in ex vivo lung perfusion, a process that involves placing lungs on a machine and monitoring their performance in isolation.
Livestream video gives the transplant center oversight throughout the ex vivo lung perfusion process.
“The lungs are ventilated and perfused—so they have fluid running through them that functions similarly to how blood would run through them—and they’re hooked up to a ventilator, and we can see over the course of three hours how they perform,” Dr. Murphy said.
If they function well, the lungs are removed from the ex vivo lung perfusion circuit, packaged on ice and sent to the recipient hospital for implantation.
“We’ve done that a number of times, which extends our ability to use lungs that we’d otherwise have to pass on. … It lets you know for sure that those lungs are going to be good,” Dr. Murphy said.
In David’s case, the donor lungs functioned perfectly.
The Spectrum Health team accepted them and prepared their patient for surgery early the next morning.
‘Secret sauce’
Cheryl, who kissed her husband goodnight and caught some sleep at a downtown Grand Rapids hotel, returned in the wee hours to await his surgery. She will always remember watching the donor lungs arrive from the airport.
The time must have been around 3 a.m.
“I’m sitting by the waiting room window and all of a sudden I see a transport vehicle come in with the lights flashing. It’s totally dark out, and I knew the lungs were in that vehicle,” she said.
“It was pretty cool.”
Throughout the morning, operating room nurses brought Cheryl reports on the progress of the seven-hour transplant procedure.
At the end, Dr. Murphy came out with good news.
“I will always remember the pride he had, the excitement he had with what he had just accomplished … and his description of how pink these lungs were and how well they were working,” Cheryl said. “That was really, really special.”
It’s one moment among many that, for Cheryl, add up to an approach that sets Spectrum Health apart.
“Spectrum has this ‘secret sauce’ of everyone giving people their full attention at the time that they’re with them. And I experienced it from the moment we were in the waiting room on our first visit,” she said.
“There are tons of little details that I can share—how I was treated, how we were respected, how people treated us as people. … To just take the time to think about those little things.”
Strong recovery
David’s recovery has been strong and steady from the start.
Cheryl noticed the difference in her husband almost immediately.
“I’d lost his essence. I mean, I’m better because of him, and I’d lost that. And it was really hard,” she said, recalling their last weeks before the transplant.
“And within 24 hours after surgery, I had the conversations back. He was talking to me about things. It was so dramatic.”
David spent about five days in the cardiothoracic critical care unit—a specialized ICU in the Spectrum Health Fred and Lena Meijer Heart Center—and a total of three weeks in the hospital before going home to East Lansing.
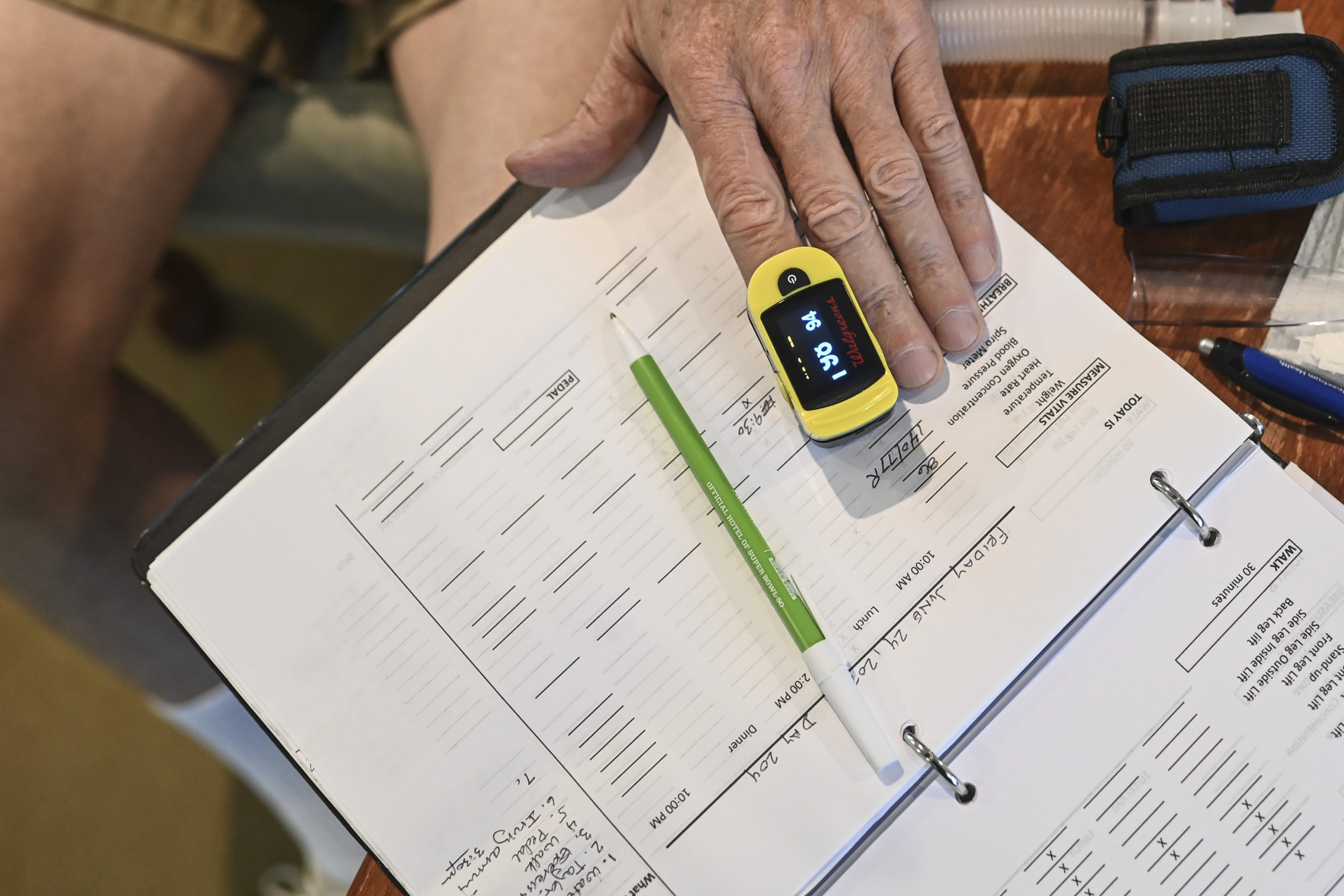
There he self-administers 15 medications a day, monitors his vital signs twice daily and arranges for weekly blood tests. He also engages in an at-home rehab program, including walking, resistance training and other simple exercises.
The fact that he remained physically active before transplantation sped up his recovery, doctors said.
Cheryl agrees.
“He could do stairs about 10 days after surgery,” she said. “By the time we left, he could easily do a flight of steps, up and down.”
For his 69th birthday this past April, David picked out a new bicycle.
“It feels great to be feeling healthy,” he said. “It’s a little bit of a challenge in that I can’t be around a lot of people right now—I keep isolated so that I avoid infections.”
But he can spend time outside with small groups of family members and friends.
And though he can’t get up close and personal with his grandchildren, who live in Colorado, he’s content with FaceTime visits for now.
“We’re hopeful that after the first year of rehabilitation is done … we can spend more time with them. It’s worth isolating now knowing that we may have tons of time later,” he said.
Cheryl is channeling her gratitude for David’s gift of life into advocacy for organ donation and participation in an online pulmonary fibrosis community.
“I am just amazed that we had the possibility to do this. They’re doing about one lung transplant a week at Spectrum—one a week. Oh my goodness, they’re doing so much to change lives,” she said.
“That we are at the point where my husband can be (lung transplant recipient) number 260 at Spectrum, it’s just amazing to me.”



























 /a>
/a>
 /a>
/a>
 /a>
/a>
WOW, what an amazing story. I think it’s amazing that other hospitals turned him down, an Spectrum took him. What an amazing team. God bless all you doctors involved.❤
Awesome! Really glad to hear that Dave is doing so well.
Very heart-warming story. Glad things turned out so well.
helped me alot prior to transplant #318 on 5/18/2023 single lung