Sue Lokker has helped hundreds of patients facing a cancer diagnosis.
A Corewell Health interventional radiology nurse, she frequently calls patients who are scheduled for needle biopsies or for line placements for chemotherapy or stem cell collection and eventually transplant.
She had rarely missed a day of work during her 35 years as a nurse until August 2021, when she underwent a hysterectomy for endometrial cancer.
“That was found very early,” she said. “It was microscopic.”
All seemed well until a couple of days before a routine post-operative appointment.
But that morning, “I noticed a big lump in my neck,” Sue said. At first, she thought perhaps she’d pulled a muscle.
Her doctor ordered an ultrasound. She’d also had a breast MRI that week, part of her routine care because of a family history of breast cancer.
“They found that my chest was full of enlarged lymph nodes,” Sue said.
A needle biopsy revealed Hodgkin’s lymphoma. “That was a huge blow,” she said.
Just like that, Sue went from caregiver to patient.
An unexpected relapse
Typically, Hodgkin’s lymphoma responds well to chemotherapy, with a cure rate of 80 to 90 percent. Sue felt optimistic going into treatment, which involved six cycles of chemotherapy every other week.
“I actually did really well,” she said, noting she experienced some fatigue but no major side effects. “I worked the whole time.”
As an interventional radiology nurse, Sue interacted with several patients with Hodgkin’s lymphoma.
“That was one of the tough things when I was working,” she said. “You’d open up a patient’s chart and you’d see, ‘Oh, their lymphoma came back.’”
A month or two after her last infusion, a PET scan revealed an enlarged lymph node. A follow-up scan revealed spots on her chest and in her armpit.
Sue, 57, returned to interventional radiology, this time as a patient. After a needle biopsy failed to produce an adequate specimen, she underwent a surgical procedure.
Her Hodgkin’s lymphoma was back.
The magic number
That’s when she met with Rupin Shah, MD, a physician with Corewell Health’s Blood and Marrow Transplant program.
The next line of defense for patients with a relapse of Hodgkin’s lymphoma is an autologous stem cell transplant. In an autologous transplant, stem cells are taken from the patient as opposed to a donor.
“It can cure a significant number of patients,” Dr. Shah said.
Dr. Shah had not met Sue before but frequently consults with interventional radiology to have lines placed prior to stem cell transplants.
“She never imagined she’d be in that position,” he said.
The BMT team determined that Sue would be an excellent candidate—she had a support system and was in good physical shape. She would need all those resources for the path ahead.
She would undergo three rounds of intense, in-patient chemotherapy.
“You use second-line chemotherapy to try to put the disease back into remission before transplant,” Dr. Shah said. “In Sue’s case it was a complete response and that gives us an indication that she’ll do well and hopefully stays in remission.”
The next phase of treatment involved collecting her stem cells. The magic number: 3 million.
To prepare, Sue had to give herself daily injections to stimulate cell production.
Each morning, her mother, Donna Grooters, would drive her from her Hudsonville home to Corewell Health’s bone and marrow transplant clinic to find out whether she had hit her goal.
“The [bone and marrow transplant] team is so wonderful,” Sue said. “I think they were as disappointed as I was every day when it didn’t happen.”
When it did, the team sent her texts with balloons and party hats. The transplant was on.
Ten days later, Sue was admitted for six days of high-intensity chemotherapy aimed at eradicating the lymphoma. It also wipes out the bone marrow and causes side effects including hair loss, mouth sores and nausea.
An emotional day
Transplant day finally arrived—on Dec. 1, 2022—which also marked the team’s 1,000th cellular infusion.
On one hand, the one to two-hour process felt “anti-climactic,” Sue said.
“On the other hand it was so emotional, because the process to get there is just so taxing,” she said.
The days after the transplant would also be taxing, when the side effects of the intense chemo entered high gear: nausea, no appetite, rashes, mouth sores and fatigue.
Her doctor and nurses gave her three jobs: Drink, eat and move.
“And have a positive attitude,” Sue said. “You think it’s sounds easy, but it’s not when you don’t have an appetite and don’t feel good.”
But Sue followed their instructions to a T, logging 70 kilometers walking the hallway of the BMT unit.
When the hospital food didn’t appeal, her husband, Dan, brought up treats from the cafeteria.
“The team, the staff on that floor, was just amazing,” she said. “It’s unlike anything I have ever seen.”
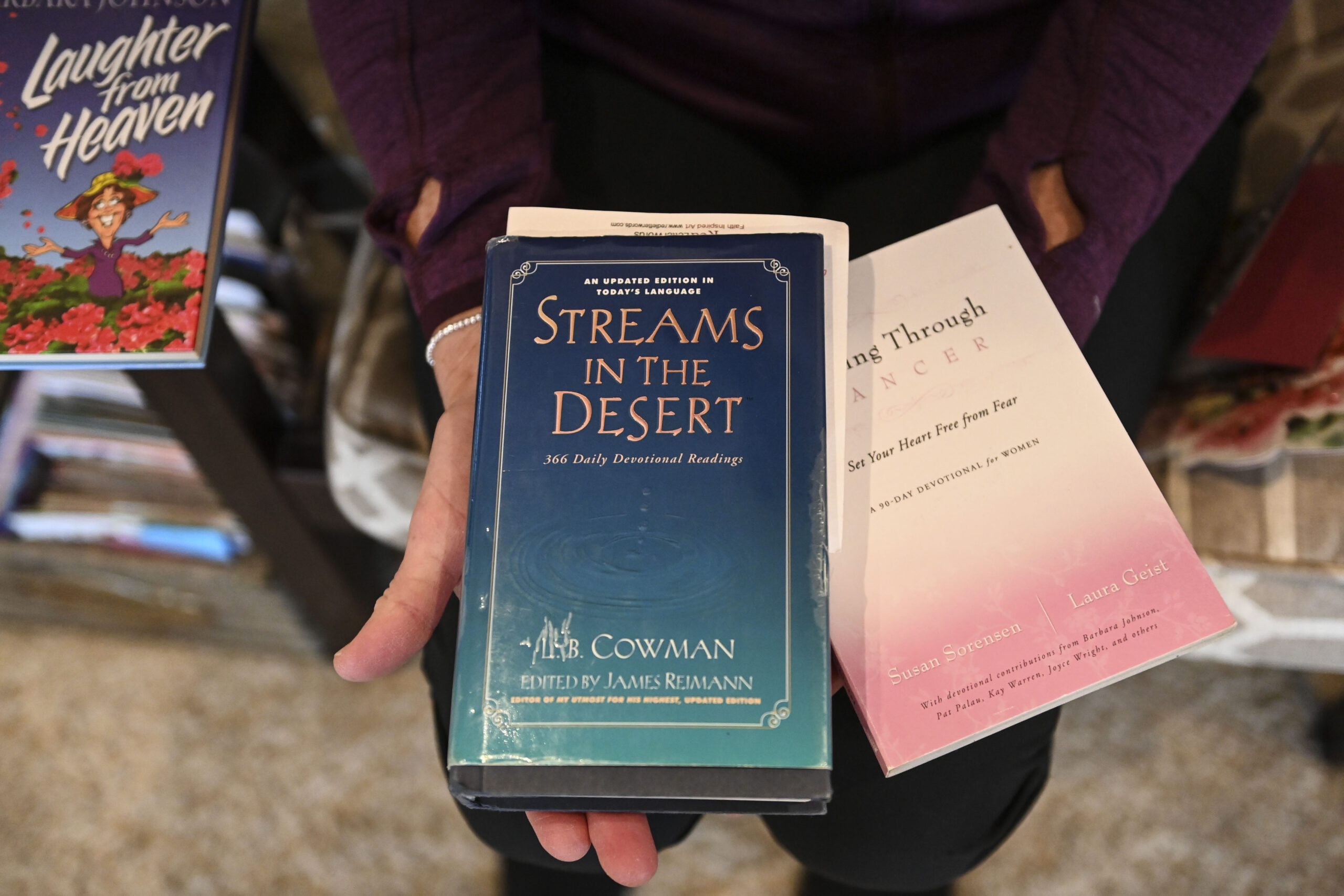
Throughout her treatment, Sue leaned on family, friends, her church community and her faith.
“It helped me through so much,” she said. “I know there is a plan. And God’s been in every detail.”
Next to her favorite chair is a box jam-packed with cards and letters from friends and family, along with a plaque that reads: “In all things give thanks.”
That sense of gratitude has buoyed Sue throughout her cancer journey.
One night, in the midst of treatment, she couldn’t sleep.
“And all I could think of was how many blessings I have,” she said.
“People ask, ‘How can you be so positive?’” Sue said. “I couldn’t think of one negative thought. All I could think of were all the blessings of my family and friends.”
A familiar wake-up call
Sue returned home after just 20 days in the hospital—short of the average monthlong stay.
She smiles as remembers the first morning.
In the hospital, the nightly soundscape consists mostly of the ding of call lights.
Her neighbors have a goats and donkeys that bray in the morning.
“I’m lying in bed in the morning and heard those donkeys braying and I said, ‘I’m home!” she said. “It’s the donkeys, not the call lights!”
“You’re really tired initially,” she said of the first weeks post-transplant. She has gradually regained strength, walking daily, feeding the donkeys, even venturing out to lunch or dinner with friends.
Sue has done “exceedingly well,” Dr. Shah said. Her PET scans show that she remains in complete remission.
The next phase of treatment involves immunotherapy infusions, given every three weeks for a year.
As she continues her recovery, now she and her mother spend time on their usual routines: grocery shopping, lunch outings and thrift shopping, instead of trips to Corewell Health.
Sue looks forward to traveling again, starting in April with a trip to Utah where she hopes to cross hiking through a slot canyon off her bucket list. She’s also looking forward to camping and gardening.
On March 2, Sue returned to work. Her personal experience, she said, “will change my practice going forward.”
“It also makes you realize how everybody’s got a story,” she said. “It makes you have more grace that you extend to other people because you don’t know what difficulty they’re going through.”


















 /a>
/a>
 /a>
/a>
 /a>
/a>
Sue- Thank you for sharing your journey with us. We are so happy you are back to work! You have something special to share as you talk with our patients, real experience to relate to others and to help ease their experience with IR.
God Bless you Sue!
What a testimony you are to so many! ✝️
Praise God from whom all blessings flow!
So thankful that you are a survivor! 💞
Hugs~
Karen (Jansma) Gerrits