Three-year-old Bethany Kerkstra was born with no scalp and missing a large portion of the top of her skull. The condition is known as cutis aplasia. She also had two holes in her heart.
She spent a significant amount of time in the Gerber Family Neonatal Center at Corewell Health’s Helen DeVos Children’s Hospital and was also admitted into the PICU before going home.
Oliver Aregullin, MD, congenital interventional cardiologist at Corewell Health’s Helen DeVos Children’s Hospital, said her brain was basically exposed at birth which was the worst of her problems from the start and would require plastic surgery to close the exposed space before attempting to close the holes in the heart.
“She had a lot of complications,” he said. “She had a skin graft and several other procedures. After our plastic surgeons colleagues got her skull healed, that’s when we started trying to fix her heart and her lungs.”
Bethany’s parents Eric and Sarah Kerkstra said she spent 8 weeks in the NICU which was difficult and traumatic for their family.
“She came home from the NICU for just 6 days, and then was readmitted to the PICU for another month,” Sarah said.
She was also diagnosed with pulmonary hypertension and has a congenital heart condition that will follow her throughout life.
“We were going back and forth to the hospital almost every day,” Sarah said. “We would send the older kids off to school and make the hour drive to the hospital where I would stay until 7 p.m. The days were very long.”
She said it is extremely hard having a baby with such a rare condition.
“Every time a new nurse came in, it was like learning an entire new lesson,” she said.
After a month in the PICU, Bethany made it home with her family.
She had several more short hospital stays leading up to her “big surgery,” as her parents put it. She eventually would have heart surgery to close her holes.
John Girotto, MD, plastic surgeon at Helen DeVos Children’s Hospital, helped reconstruct Bethany’s head in partnership with pediatric neurosurgeon Marian Bercu, MD.
“These holes in the skull are usually the size of a nickel, but Bethany’s was almost the entire top of her head,” Dr. Girotto said. “It was a complicated procedure, but her family came to the right place as our team is skilled in remedying these situations.”
A ‘doughnut’ shaped device
Bethany was also diagnosed with pulmonary hypertension and suffered from fainting episodes and seizures. The fainting was caused by the pressure in her lungs being too high which made her heart stop being able to pump blood.
She was on three medications to treat it, with no luck.
Physicians performed several heart catheterizations prior to surgery in April of 2020. Dr Neal Hillman repaired two holes in her heart, one an atrial septal defect (a hole in the wall that divides the upper chambers of the heart) and the other ventricular septal defect (a hole in the wall that separates the two lower chambers of the heart).
When Bethany was 2 year old, Drs. Aregullin and Vettukattil performed a cardiac catheterization to implant an investigational device in her heart. The investigational device, Atrial Flow Regulator (AFR), opens the upper chambers of the heart, and through a hole, doctors can decompress pressure on the heart.
This technique had been used in Europe but has not been approved by the FDA, so Bethany was the smallest and youngest patient to have this procedure in the United States.
Dr. Aregullin received special compassionate-use clearance from the FDA and placed the Atrial Flow Regulator in Bethany’s heart in April 2022.
“The device is small, it was put in through a heart catheterization,” Dr. Aregullin said. “It looks like a tiny doughnut and it helps shunting blood between the two upper chambers of the heart.”
Bethany’s family also applied for a double lung transplant, but for now doctors want to wait and see if medicine and the additional shunt through the AFR device will help her body reach better oxygen levels and manage her pulmonary hypertension.
Fortunately, Bethany’s mom said she hasn’t passed out since the device was implanted and seems much better.
“When patients get too much pressure in their lungs, they have difficulty breathing, can go into cardiac arrest and can even die,” Dr. Aregullin said. “She never got to that serious of a situation as the AFR device helped keep that from happening.”
Doctors have tried different medications since placing the device with good results.
And after the successful surgery and months of recovery, Dr. Girotto and his team were able to stabilize her head and continue plastic surgery.
‘Living her best life’
Bethany’s mother Sarah said she lives a very full life although she is slightly limited. She can walk, run and play, but she’s almost always out of breath.
“When she is panting, that is almost her normal level of breathing,” Sarah said. “She’s a typical 3-year-old with a little attitude and sweetness all in one. She is learning the alphabet, numbers, letters and colors, but hasn’t been too vocal just yet.”
Lucky for Bethany, she has two older siblings who happily do the talking for her, Olivia, 10, and Henry, 8. Two Doberman siblings, Rocky and Ruby, round out their family.
They have home schooled the kids since 2020, as every little illness can become a serious setback for a child with a compromised immune system.
Sarah said Bethany has some developmental delays, motor skill issues and speech delays, but is still fairly active.
Bethany and her family live on 15 acres of woods where they enjoy outdoor activities like riding four-wheelers and nature play.
“She loves splashing around and playing the dirt too,” Sarah said. “Along with learning to read and looking at books.”
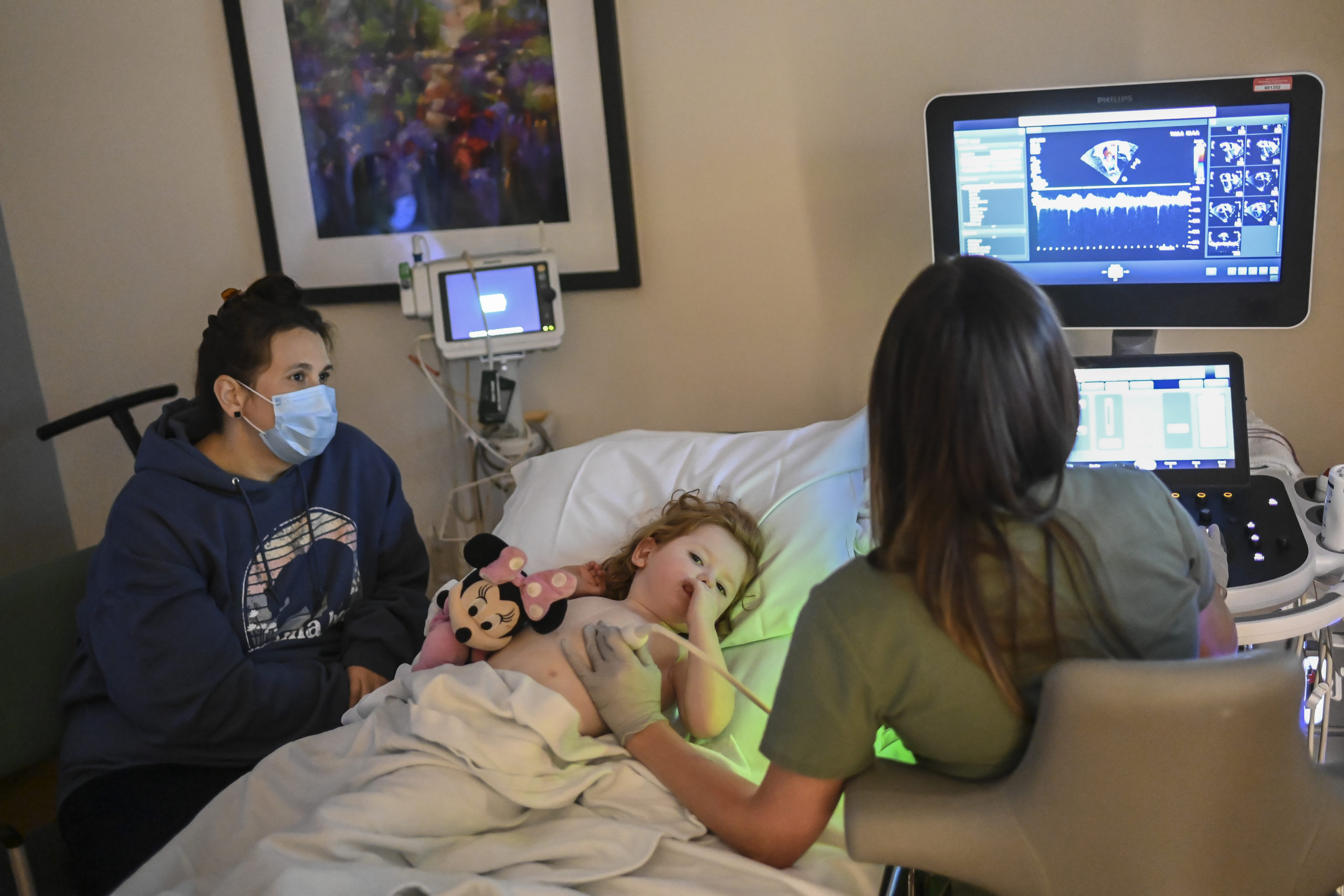
Bethany also loves Minnie Mouse and Hot Wheels.
Dr. Aregullin recently checked in with the family and said this is the first time she has been above the 50th percentile for growth and development.
“She is doing great,” he said. “This is definitely a milestone for her.”
Bethany is currently on three powerful medications for hypertension.
“Right now she does not have any significant concerns for heart failure,” Dr. Aregullin said. “She is the smallest patient we have used this device on. And seeing her almost nine months after … from what I see and what I hear, she is doing much better.”
He said her oxygen levels are essentially normal too.
“Right now she is living life completely like a normal 3-year-old,” Sarah said. “Her legs are a little weaker than other kids. But other than that, she is just living her best life.”



































 /a>
/a>
 /a>
/a>
 /a>
/a>
Thank you Rick for writing this story! Thank you to everyone at Helen Devos Childrens hospital for everything you have done for my beautiful daughter Bethany! We are so very blessed!
I would love to talk to Bethany’s parents! I’m a 62 year old congenital heart patient born with heart rate of 34 bpm with 2 holes in my heart. I was the youngest person to get a pacemaker in 1962 when it was still experimental. I’ve lived a full life with normal activities, I hope this is encouraging!