On May 22, 2022, the Tomaszewski family planned to kick off summer splashing in their pool with friends.
Instead, they ended up in Corewell Health’s Helen DeVos Children’s Hospital emergency department with their oldest daughter, Claire “Gigi” Tomaszewski, who suffered a severe anaphylactic reaction.
The culprit: a walnut hidden in a brownie.
Now, the family is eager to share the lessons they learned that day—and express their gratitude for Erica Michiels, MD, the pediatric emergency medicine doctor who treated Gigi.
“Dr. Michiels is a hero,” Jane Tomaszewski, Gigi’s mother, said. “She literally saved my daughter’s life. If she hadn’t stepped in and recognized the care that she needed, we would have had a much more terrible outcome.”
The Tomaszewskis, who live in Ada, Michigan, knew Gigi, now 7, had a walnut and pecan allergy.
But her previous reactions had been mild.
At age 2, Gigi had a lick of butter pecan ice cream, which caused her to cough and cry. Benadryl eased her symptoms. Another time, Gigi broke into hives after eating ham that had touched walnuts on a charcuterie board.
They were concerned, so they took her to an allergist. Allergy testing revealed the walnut and pecan allergy, so they eliminated those items from her diet and started carrying the epinephrine doctors prescribed, in the form of an epinephrine auto-injector.
It’s a medical device used to quickly deliver epinephrine in the event of a severe allergic reaction, called anaphylaxis.
They never used it—until that day in May.
‘She was going into shock’
Jane said friends they had invited to the pool brought brownies containing walnuts, not knowing Gigi was allergic. Gigi ate a few bites of her brownie and immediately knew something was wrong.
She said her mouth felt itchy, so Jane went inside to get Benadryl. As she looked up the correct dosage, Gigi’s condition worsened. She broke out in hives and vomited, then started vomiting blood.
Jane called for her husband, Dan, and together they administered the epinephrine to Gigi, injecting it into her thigh as prescribed.
“We had never done this before,” Jane said. “We thought, ‘Isn’t she supposed to be getting better? How long does this take to work?'”
Since it was Sunday afternoon, they called their pediatrician’s on-call service and then headed to urgent care.
They piled into the car as quickly as they could, still wearing their swimsuits.
“Gigi was barely lucid and limp,” Jane said. “I held her in the back seat because we couldn’t put her in the car seat. We were just flooring it there.”
At the urgent care, a physician’s assistant immediately called 911. An ambulance transported Gigi to the Helen DeVos Children’s Hospital emergency department.
Soon after their arrival, Dr. Michiels walked in the room. She knew about Gigi, as the EMTs from the ambulance had called on their way to the children’s hospital.
Dr. Michiels was very concerned by what she saw: Gigi’s skin was bright red. Even more alarming, her face, hands and feet were blue.
“She was experiencing circulatory collapse from the anaphylaxis,” Dr. Michiels said. “She was going into shock.”
Dr. Michiels immediately ordered another dose of epinephrine.
After that, Gigi needed even more. The doctor put Gigi on a continuous intravenous drip of epinephrine, something she has only needed to do a few times in her entire career.
“She was having a severe ongoing case of anaphylaxis that was resistant to standard treatments,” Dr. Michiels said. “Generally, kids respond right away to that first shot of epinephrine. It’s kind of like a miracle. But Gigi needed a continuous epinephrine drip to get this turned around for her.”
Making changes
Anaphylaxis has many symptoms: hives and itching, low blood pressure, weak and rapid pulse, nausea, vomiting, dizziness, fainting and more, Dr. Michiels said.
But perhaps the most commonly known symptom is the airway swelling shut, causing coughing, wheezing and trouble breathing. Gigi was experiencing other serious symptoms, but not that one.
“The one that terrifies people the most, and rightfully so, is that the airway is going to swell shut,” she said. “Because Gigi was alert, she was conversing with us and her airway was OK. That gave people a little bit of false sense of security.”
A big advantage for Gigi: She was in an emergency department that treats children.
“Kids don’t tell you what’s going on,” Dr. Michiels said. “I have the experience to look at a child and know something isn’t right. It takes time and experience and repeated exposure to what a little kid going into shock looks like.”
She explained that children often compensate better than adults because, generally, they have healthy hearts.
“Kids hang on, until they don’t,” she said. “They look better longer than adults, until they fall off a cliff. Gigi was heading for the cliff, but she was compensating very well.”
Once the care team stabilized Gigi in the emergency department, Dr. Michiels transferred her to the pediatric intensive care unit for 24 hours for more treatment and monitoring.
She visited Jane, Dan and Gigi later that night.
Dr. Michiels said she’ll always remember the look on Dan’s face as they talked about what Gigi had experienced.
“I could see in his eyes that he realized that he almost lost Gigi that day, but he didn’t,” Dr. Michiels said. “It’s one of those things I will never forget.”
Jane hopes other parents can learn from their experience.
“I was totally underprepared,” Jane said. “I knew she was allergic, and we had an EpiPen. But I didn’t know that when you give the EpiPen, it’s consumed quickly in the body and she might need more.”
Since then, the family has made changes.
Under the care of Amanda Holsworth, DO, an allergist with Helen DeVos Children’s Hospital Allergy and Immunology, and her partners in the practice, Gigi underwent updated allergy testing.
It confirmed she’s allergic to walnuts and pecans. They opted to completely eliminate all tree nuts from Gigi’s diet.
Dr. Holsworth is pleased to see Gigi and her family managing everything so well.
“They are doing a wonderful job,” she said. “They’re very vigilant. Gigi is so responsible and asks great questions. She’s so bright and she does a wonderful job—for being 7 years old—of managing her food allergy.”
‘And now we know’
At a recent visit, Dr. Holsworth said they discussed potential therapies that would hopefully reduce the severity of Gigi’s reaction if she experiences another accidental ingestion.
Jane said they’ve been telling everyone they know about the severity of Gigi’s allergy.
“We weren’t that careful,” Jane said. “And now we know.”
They take many more precautions at home and in public.
For instance, on a trip south to Georgia and Florida, where pecans are very common, Gigi wanted pancakes or waffles for breakfast one morning. At the first restaurant they went to, they learned that pecans are regularly cooked on the griddle.
So they headed to another restaurant, where they learned the same thing. They ended up at a fast food restaurant where there were no nuts.
“It’s a risk we’re just not willing to take,” Jane said.
At school, where Gigi is in second grade, she now sits at a nut-free table for lunch. She has an epinephrine auto-injector in the school office, as well as in her backpack and with her at all times. She even carries it the short distance down the hallway to the lunch room.
“She said, ‘I like having it with me,’” Jane said. “She understands that she went through a really, really tough thing.”
They processed it after that day, as Gigi was able.
“At one point a couple days after the incident, Gigi said, ‘Mom, everything was purple. When were we in the car on the way to urgent care, everything was purple. The sky, the trees were purple,’” Jane said.
‘It’s a really special thing’
Both Dr. Michiels and Dr. Holsworth urged families that have been prescribed an epinephrine auto-injector to be sure they always have it—and to use it if needed.
“Families are afraid to use it,” Dr. Michiels said. “If you think you should give it, you should give it. There’s no downside. It’s not going to harm them. The biggest harm is not giving it.”
Then call 911, or drive quickly to an emergency department.
After administering the epinephrine, if the patient is not improving, Dr. Holsworth said, you may give the second dose.
Two auto-injectors come in each prescription and they should always be kept together. The second one can also come in handy if something goes wrong in administering the first one.
Dr. Holsworth said patients need to be seen by a medical professional, even if the epinephrine appears to be working.
Both doctors reminded families that allergic reactions can change over time.
“Past reactions are unfortunately not predictive of future reactions. That can be a good or a bad thing,” Dr. Holsworth said.
If an initial reaction was severe, it doesn’t mean other reactions will be as severe. On the flipside, a previously mild reaction may falsely reassure families that their child will not have a severe reaction.
“Any reaction can, by definition, be severe and life-threatening,” Dr. Holsworth said. “That’s why you have to have epinephrine.”
The proper actions are outlined in a plan created by a child’s allergist, called a Food Allergy and Anaphylaxis Emergency Care Plan. Dr. Holsworth urges families to become familiar with it and to ask questions at appointments.
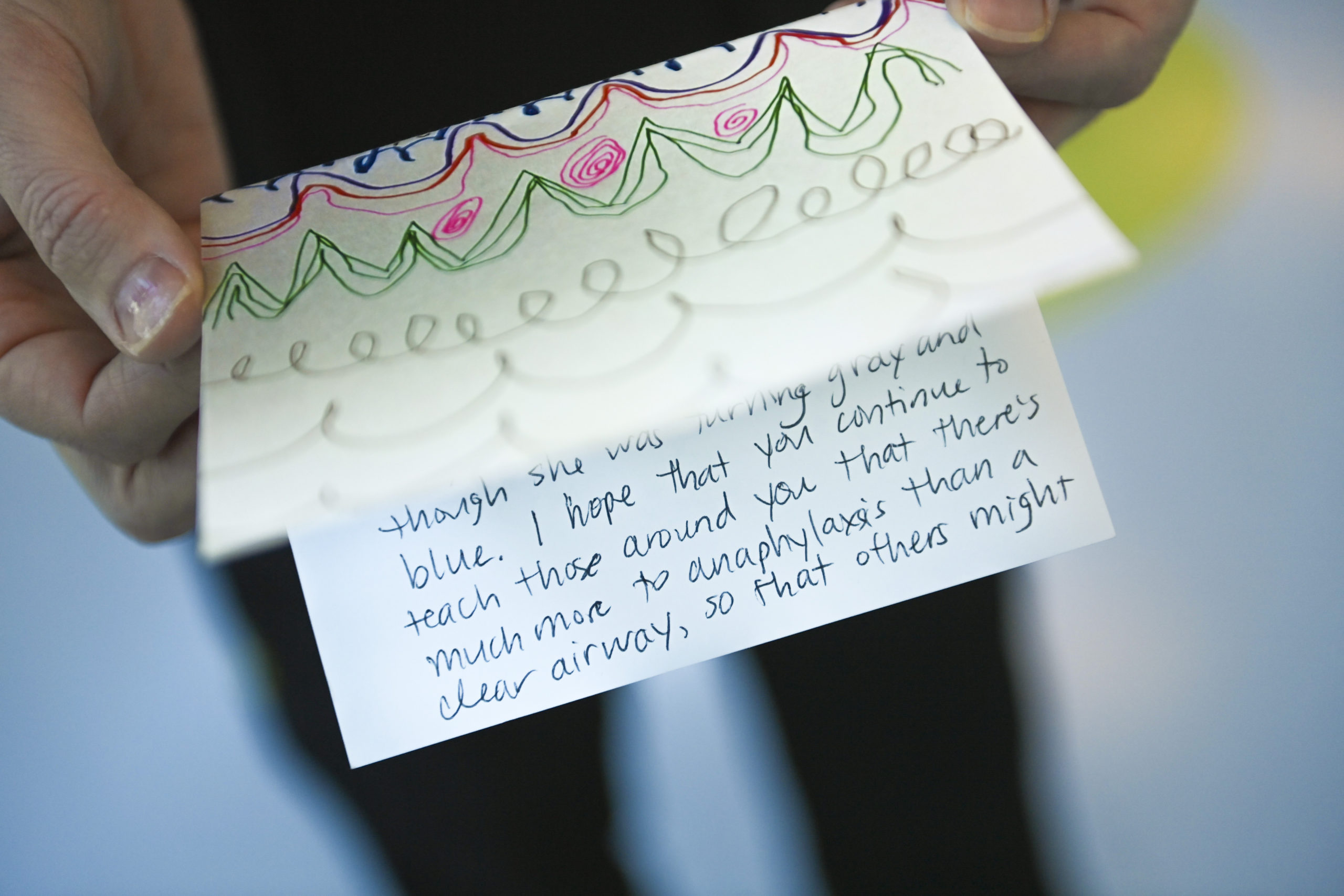
After their experience, the Tomaszewskis wrote Dr. Michiels a thank you note, handwritten on a card featuring Gigi’s artwork.
The doctor keeps it hanging above her home office desk, alongside pictures of her family.
“It is worth everything. It’s got a special spot in my office,” Dr. Michiels said. “It’s a good reminder, especially in emergency medicine. We meet families on the worst day of their lives. It’s a lovely reminder to look over and know there’s not only someone who appreciates what I did, but a little life in the world that I had a hand in.”
It’s one of the greatest rewards of working in pediatrics, she said.
“Knowing there’s this little girl who has her whole life ahead of her because our team was there that day to treat her,” Dr. Michiels said. “Who knows what she’s going to grow up and do and be in the world. It’s a really special thing.”



















 /a>
/a>
 /a>
/a>
 /a>
/a>
My friend’s daughter has a tree nut allergy and had a reaction to her new bed. The headboard was treated with a wood polish containing nut oil.
Wow! It’s not every day I stumble across an old high school classmate in this newsletter. A nice reminder that almost every health issue featured on HealthBeat could happen (or has happened) to someone we know.
Dan, I’m sorry your family went through something so scary, but I’m glad it resulted in a positive outcome! And kudos for spreading the word about anaphylaxis and how people can equip themselves to better handle it.