Like most babies, Ollie Lott came into the world crying, wiggling and naked as God made him.
But he brought something extra also—a coiled tube stuck out of the pale pink skin of his little belly.
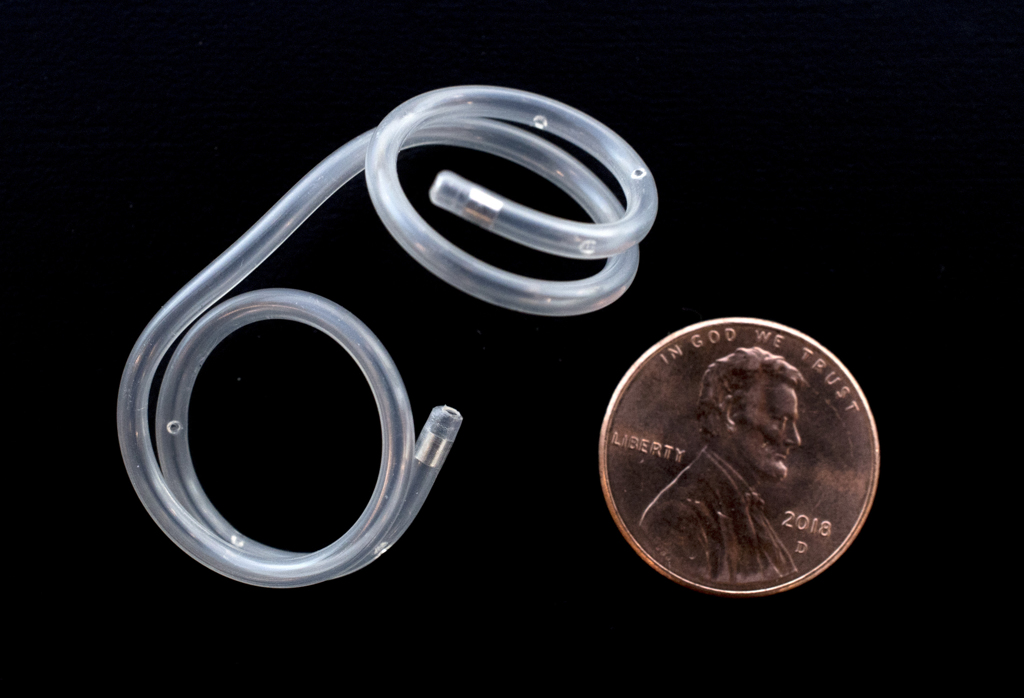
The catheter, surgically implanted 14 weeks earlier, helped him overcome a birth defect that could have been fatal.
“It’s amazing,” said his mother, Kimberly Lott, as she cuddled Ollie, now a cooing and smiling 10-week-old baby.
“I didn’t know any of this stuff existed. I didn’t know people could do surgeries on babies while they were in the womb.”
The procedure certainly is rare—as is the birth defect, said Vivian Romero, MD, a Spectrum Health maternal fetal medicine specialist.
For Ollie, timing and technology came together to make possible the operation, and its happy outcome.
Ultrasound reveals a problem
Kimberly and her husband, Anthony, had no clues of the drama ahead as they prepared for the birth of their second child. They looked forward to welcoming a younger sibling for their 5-year-old son, Elliott.
At 20 weeks, Kimberly had a routine ultrasound near her home in Holland, Michigan. Because the baby’s kidneys and bladder were enlarged, Kimberly’s doctor referred her to the maternal fetal medicine specialists at Spectrum Health.
A few days later, the Lotts visited Dr. Romero and she performed another ultrasound. It, too, revealed enlargement of the bladder, kidneys and the ducts that connect the two.
“It looked like the baby had an obstruction, most likely below the bladder,” she said.
That tiny piece of plastic saved his life.
It was hard to get a detailed picture. A developing baby generally floats in amniotic fluid, which aids visualization of the anatomy. But in Ollie’s case, there was essentially no amniotic fluid. Dr. Romero could not even see if the baby was a boy or girl.
The lack of fluid can lead to damage of the urinary tract, kidneys and lungs.
“The baby releases urine to the amniotic cavity, and then the baby swallows and breathes the fluid, allowing the lungs to develop,” Dr. Romero explained. “Low amniotic fluid can result in underdevelopment of the lungs—pulmonary hypoplasia, a life-threatening condition.”
In the early stages of pregnancy, the placenta creates the amniotic fluid. The kidneys take over the job after week 17.
By retaining urine, the blockage in Ollie’s bladder disrupted that cycle. Later tests showed he had posterior urethral valves, which means he had extra flaps of tissue in the tube through which urine leaves the body.
The rare condition occurs in 1 in 8,000 to 1 in 25,000 live births of baby boys, said Alejandro Quiroga, MD, a pediatric nephrologist with Spectrum Health Helen DeVos Children’s Hospital.
Depending on the degree of the obstruction, the condition can be fatal.
‘We will try it’
The Lotts, reeling from the news of their baby’s prognosis, struggled to comprehend the options laid out for them. They could wait and let nature take its course, loving their child for his brief life on earth.
Or they could see if a shunt could be placed in utero in the bladder.
“It sounded kind of far-off,” Kimberly said. “I didn’t know if that was going to work. It seemed weird. But we said we will try it.”
First, they had to see if Ollie was a candidate for surgery. The maternal fetal medicine team had to make sure Ollie’s kidneys still worked and could produce urine. The surgery would not benefit him if the kidneys were so damaged they could not function.
I was so scared. I didn’t want to get my hopes up.
Dr. Romero performed a bladder tap, using ultrasound to guide her as she placed a long needle through Kimberly’s uterus and into Ollie’s bladder.
From that tiny sac, she withdrew about a teaspoon of urine.
“I felt it. It wasn’t good,” Kimberly said. “That first bladder tap was the worst. My whole uterus contracted. I was crying. I was upset. I was swearing.”
And most difficult of all: She had to repeat the bladder tap the next day. The second test would show if the bladder filled with urine again, indicating Ollie still had functioning kidneys.
Kimberly didn’t hesitate.
“I wanted to do everything I could do,” she said.
Daring to hope
The tests showed good renal function, so Dr. Romero performed the surgery. Kimberly was 23 weeks pregnant.
Using a larger, hollow needle, Dr. Romero placed the shunt into Ollie’s grape-sized bladder.
The tube, called a pigtail catheter, curled into a loop on each end. She placed one end coiled up inside his bladder. The other end looped in a circle outside his body, along his belly.
Urine flowed through the catheter from the bladder to the amniotic sac, bypassing the blockage.
For the rest of the pregnancy, Kimberly returned for repeated follow-up tests to make sure the catheter remained in place. Babies often manage to pull them out.
With each visit, Kimberly worried about whether the shunt still worked, whether her baby was growing.
“I was so scared,” she said. “I didn’t want to get my hopes up.”
As the weeks progressed without problems, she began to be hopeful. She stopped researching palliative care options and started reading about kidney issues. A few weeks before the delivery date, she finally allowed herself to buy a few baby outfits for him.
Throughout the pregnancy, the maternal fetal medicine team also monitored the growth of Ollie’s chest.
“We were all worried about how his lungs were working,” Dr. Romero said. “We noticed his chest was growing, so we hoped his lungs were growing, too. But we wouldn’t know until the baby was born.”
They planned to induce labor at 37 weeks. But three days before the delivery date, an ultrasound showed a drop in fluid levels. The catheter was not visible on the scan. The maternal fetal medicine specialists decided to deliver him that day.
That night, Dr. Romero performed a C-section, and Anthony Oliver Lott was born. He weighed 6 pounds, 15 ounces.
“He came out and just started wailing,” Kimberly said. “It was such a relief to us.”
On his belly lay the coiled catheter that had been so elusive on the last ultrasound.
“Everyone was pointing at it and saying, ‘There it is! It’s in there,’” she said.
It didn’t take long to see it was still doing its job.
Ollie’s lungs managed to avoid major damage. In the children’s hospital neonatal intensive care unit, he didn’t need to be on oxygen.
His kidneys sustained major damage, but that had been expected.
‘We can deal with that’
Kimberly gave Ollie a bottle as her son Elliott played a computer game nearby. She talked about the challenges her infant son has already faced in his short life.
Five days after birth, he underwent surgery to remove the valves that blocked his urethra. Tubes were placed in his kidneys to drain urine from them. And he had a port placed so he can have dialysis in the future.
He will need a kidney transplant eventually. Kimberly hopes she will be able to give him one of hers.
He also has a feeding tube to make sure he gets enough nutrition. Children with kidney disease often have poor appetites, Kimberly explained.
Ollie’s health challenges don’t faze her. She just marvels at her son’s bright eyes and alert gaze, his wiggly arms and legs, his sweet smile.
“When he came out and all that was really damaged was his kidneys and urinary tract system, I said, ‘This is manageable. We can deal with that.’ There’s lots of kids in the world who have kidney disease and they are fine.”
She looks to his future with hope.
“He’s a little fighter,” she said. “He has been since the beginning.”
She opened a small bottle and tapped out a plastic tube, curled at both ends: the catheter that had been implanted in utero.
“It saved his life,” she marveled. “That tiny piece of plastic saved his life.”
Ollie’s progress is also deeply rewarding to his physicians.
“This is why you go into medicine, because you want to save lives,” Dr. Romero said. “You want to do good for people.”
She credited Kimberly and her doctor with seeking specialized care as soon as the problem with his bladder appeared. The timing was crucial to the success of the shunt surgery.
Dr. Quiroga praised the Lotts and their vigilance in managing Ollie’s complex health issues, during pregnancy and after birth.
“The family is awesome,” he said.
As for Ollie, he said, “He’s doing great. He’s surprising us. He’s keeping us busy but he’s doing well.”





























 /a>
/a>
 /a>
/a>
 /a>
/a>
Wow, what amazing things God has given to the doctors!! So proud of these parents for their courage and bravery as well!!
What a mindblowing story! Cannot imagine the stress along the way, but so happy for their family and the Beautiful Ollie.
Truly an amazing story! Thank you for being a Health Beat reader and for your kind comment, Tracey!
Brought me to tears. What a blessing!
Thank the Lord for blessing this baby and these wonderful doctors with such talent! I personally met Dr. Romero before and she is very sweet, kind and caring. My best friend was a patient of her’s 3 years ago and thanks to her and her team – she now has a healthy and strong boy.