December 1 started like any other day for 76-year-old Jerry Densmore–until he became among the first people in the country to have a blood clot removed from his brain using a brand-new device.
“I was standing at the front door when I fell up against the screen door,” said Densmore, a retired plumber who lives in Bitely, Michigan. “I told the wife, ‘I just need to sit down.’ But she never listens to me anymore. And it’s a good thing. She probably saved my life.”
Densmore’s wife, Cheryl, immediately noticed the left side of his face was drooping and his speech wasn’t quite right.
Confident he was having a stroke, she called an ambulance, which rushed him to Big Rapids Hospital then on to Butterworth Hospital in Grand Rapids.
That’s when Director of Vascular Neurosurgery Justin Singer, MD, stepped in and put to use the Zoom RDL device, making Densmore one of the first people ever to have a blood clot removed with it.
A nimble approach
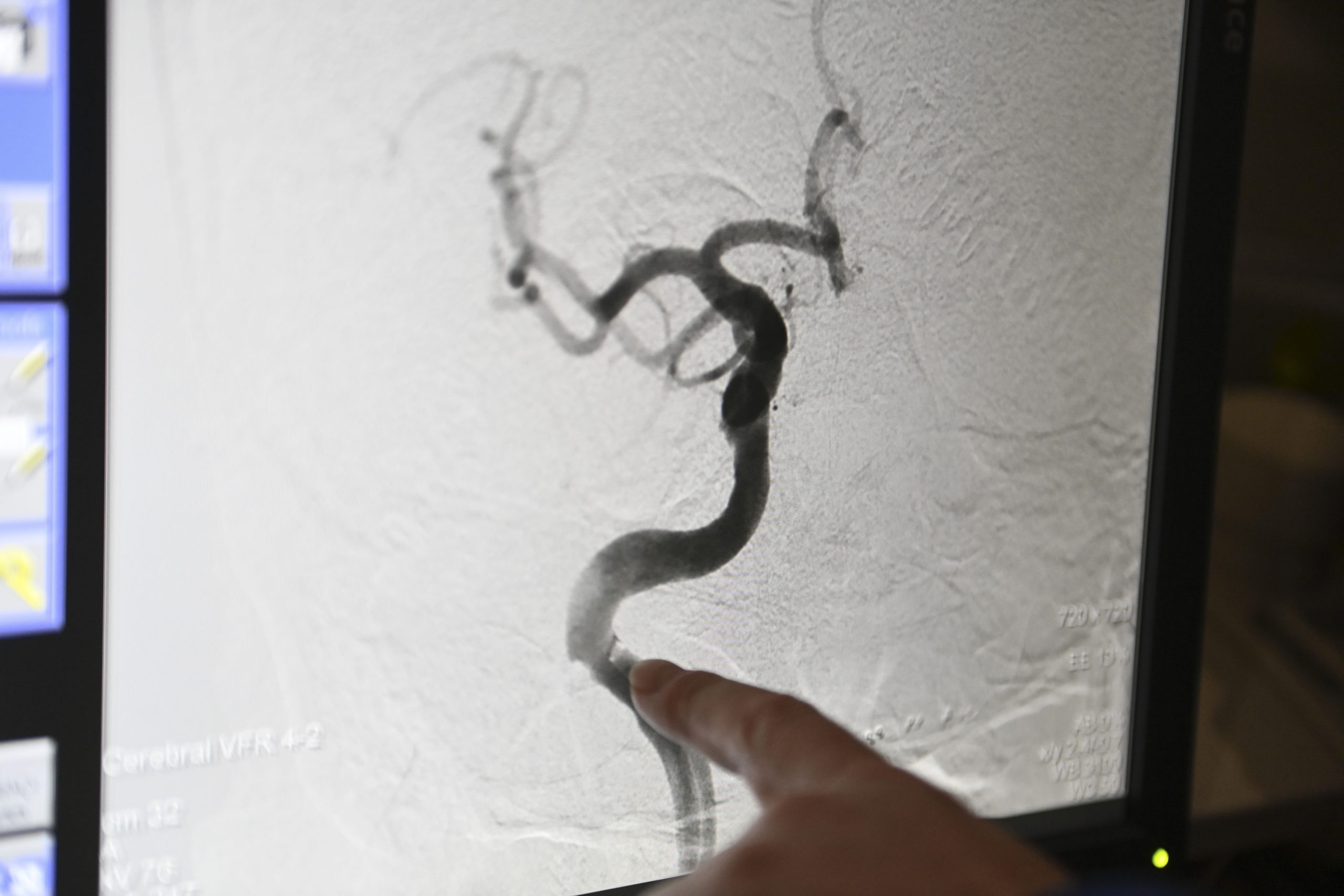
The device is used during a mechanical thrombectomy, a minimally invasive procedure that allows a surgeon to thread a catheter through one of a patient’s main arteries and up into the brain to capture and remove a blood clot.
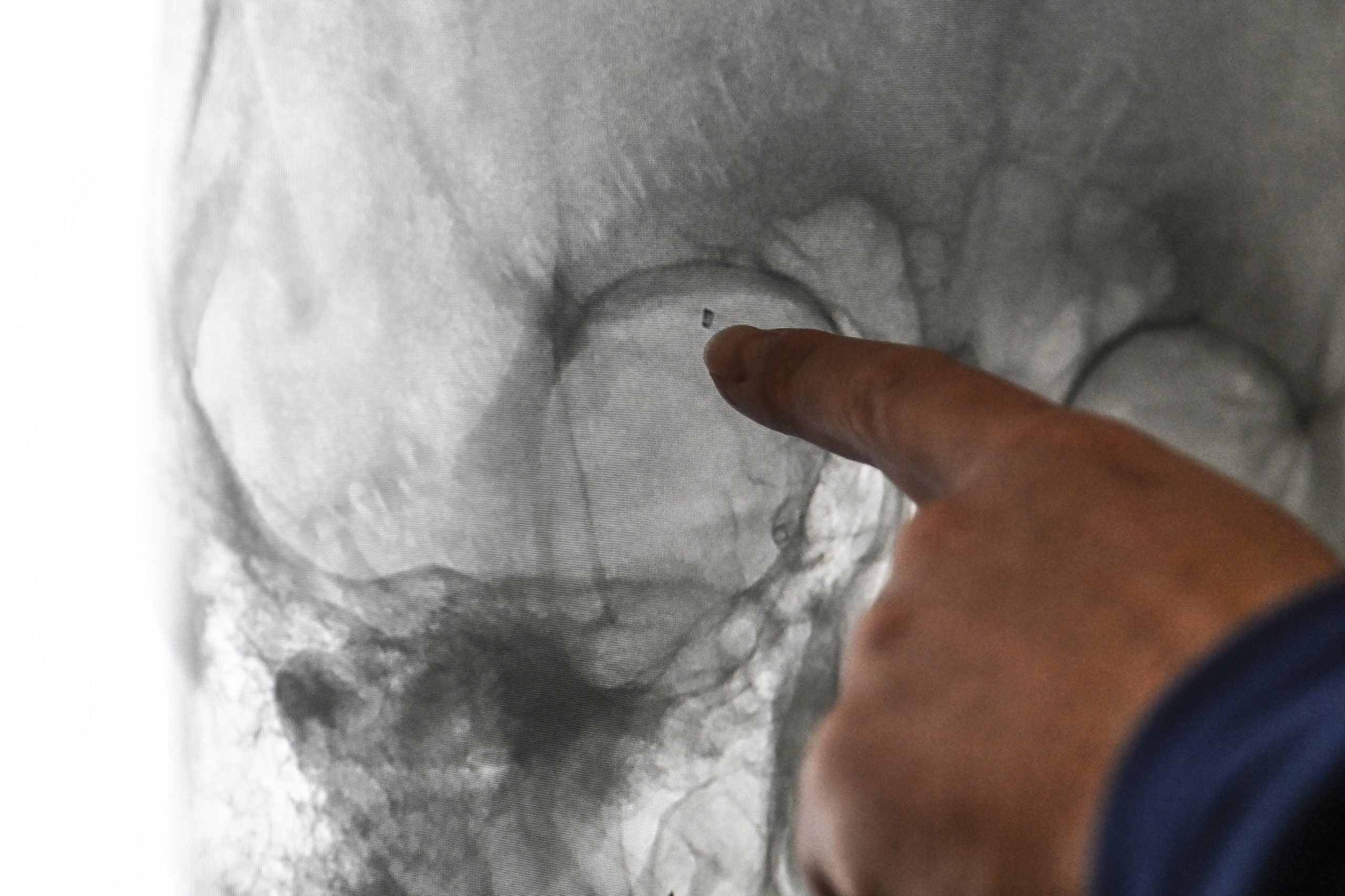
In Densmore’s case, the clot was on the right side of his brain, cutting off the blood flow necessary to keep his brain alive and fully functioning.
The Zoom RDL allowed Dr. Singer to gain access through the radial artery in Densmore’s hand. Most commonly, a thrombectomy goes through a patient’s femoral artery, accessed in the leg.
And while Dr. Singer and others previously have performed thrombectomies through the radial artery, the tools they used weren’t designed for that purpose.
The Zoom RDL is longer than a traditional catheter and has a unique tip, “providing a more systemic approach to radial access. It gives me more flexibility and is less clunky” than using a catheter designed for the femoral artery, said Dr. Singer, who was the first neurosurgeon in the country to use the device to treat a stroke.
“It’s like framing a house. You need a good, stable foundation to build the rest of your procedure on,” he said. “Having this new technology will help us help more patients.”
But radial access isn’t for everyone, Singer said. Femoral access is generally faster—unless vessels are twisted, which is a common occurrence as we age.
Maneuvering through all those twists and turns takes time, which is at a premium when dealing with a blood clot that is blocking the flow of oxygen-rich blood to the brain.
“We lose hundreds of millions of brain cells every minute there’s a blockage, so any tool we have to move more quickly is important,” Dr. Singer said.
He added that scans provided in advance of the procedure give him a good idea of the patient’s anatomy and help him decide how best to proceed.
Restored in minutes
Densmore doesn’t remember anything about the procedure, which took about 18 minutes and restored blood flow to “near normal,” Dr. Singer said.
Shortly after, when he transferred into a patient room, he was able to move and communicate without much difficulty.
Another advantage to radial access pertains to post-operative recovery time.
Densmore described the entry point on his hand as “just like a little scratch, not much different than having an IV.”
Conversely, when the access point is the femoral artery, patients must lay flat for about six hours after surgery so the artery can close and healing can begin.
Many of his patients receive clot-busting medications, “so there is a risk for substantial blood loss. The risk is low, but you don’t want that to happen even one time,” Singer said.
Right before Densmore concluded his brief hospital stay and headed home, doctors implanted a cardiovascular monitor just above his breastbone.
It links to his phone and sends regular updates to ensure his heart is pumping normally. A chaotic rhythm can cause blood clots.
Two months later, he graduated from in-home occupational and physical therapy and he’s looking forward to fishing once again on Nichols Lake this spring and summer.
“I was having problems with my balance at first, but gradually that disappeared. I’m back on my feet again and everything is back to normal. I’d say I’m 98 or 99%,” he said.
Still, he thinks about what happened and how the outcome could have been so much different if his wife and the medical professionals hadn’t taken quick action.
“People need to pay attention to this. If you have symptoms, and they are not hard to learn, get your tail to the hospital as soon as possible. The sooner the better,” he said.


















 /a>
/a>
 /a>
/a>
 /a>
/a>
Dr. Singer saved my daughter’s life when she had a stroke 3 years ago at 14. I am forever grateful for him, his wisdom and courage.
The radial artery is accessed in the wrist, not “the hand”!